Find the latest COVID-19 news and guidance in Medscape's Coronavirus Resource Center.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I'm Dr F. Perry Wilson.
One of the things that has really bothered me about COVID-19 is the dramatic variability in presentation, from being asymptomatic to having sniffles, complete respiratory failure requiring ECMO, and, of course, death. I've seen all of these firsthand at this point. And sure, we know that there are risk factors for bad outcomes, such as older age and comorbidities. But ask any of us who have cared for these patients and we'll tell you that there is clearly other stuff going on. I've seen a 35-year-old man with no comorbidities fighting for his life on ECMO.
It seems logical that genetics may play a role here, but those studies are just in the early phases. Nevertheless, some tantalizing clues are emerging—and some from really unlikely places.
Okay. A couple of months ago, my family did tests to figure out our blood type. We did this for no scientific or medical reason; we were bored, stuck at home, wanted some fun science-y stuff to do with the kids, and found some cheap kits on Amazon.
I am type O. My wife, type A.
And that was that. Until I started seeing that blood type may be associated with the risk for coronavirus infection and death from COVID-19.
This supposition immediately raised red flags for me. Correlating blood type with various outcomes has long straddled the border between regular science and pseudoscience—and often had a racially tinged flavor. I am pretty sure blood type does not correlate with various personality traits, for example. So why would blood type dictate susceptibility to a respiratory virus?
But, since I am often wrong and love to find out when I'm wrong, I looked into it. And I honestly think there may be something here.
Caveats: Data are really limited, and studies are sort of trickling out in preprint form and in various esoteric journals. But I'll point out a couple that hold water for me.
The first, a preprint out of China, looked at just over 2000 COVID-positive individuals and reported that there was a higher infection rate in people with type A blood.
What you see here is that there was a higher-than-expected rate of individuals with blood group A diagnosed with COVID-19 than in the general population.
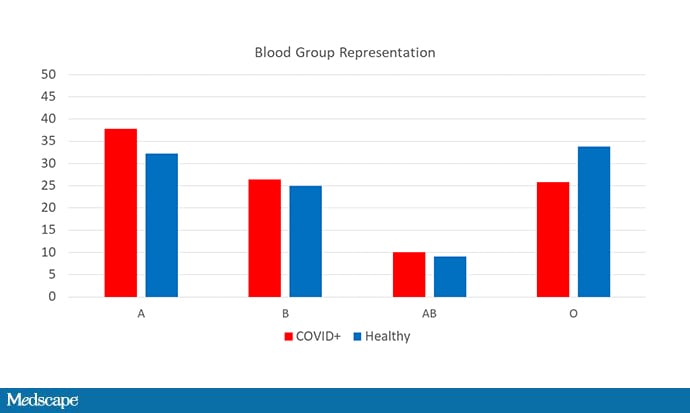
Conversely, fewer-than-expected individuals with blood group O appeared in the pool of those infected. Similar results were seen when the analysis was restricted to the 206 individuals who died from COVID-19. Again, blood group A was overrepresented.
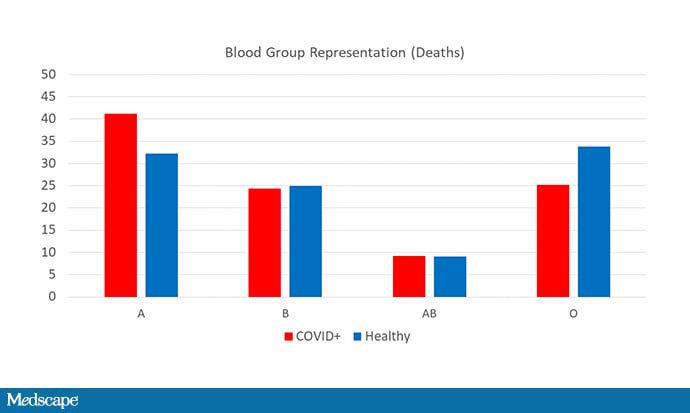
One study, especially in preprint form, is never definitive, but we now have this study from New York City to add to the data. This study looked at 1559 patients who were tested for COVID-19; 682 were positive. And check out the distribution of blood types in the positive vs negative groups.

Again, blood group A is overrepresented and blood group O is underrepresented among the infected.
The commercial DNA testing company 23andMe has reported that their analysis of over 750,000 genomes shows a similar pattern by blood group. They haven't published their data yet, but you can see here that the self-reported infection rate was lower in type O individuals and higher in type A individuals, though overall rates are still low.

These data don't come totally out of the blue. Back in the SARS era, a Hong Kong study reported that type A individuals were at higher risk for infection from that coronavirus.
But what's the biological rationale here? Even if we believe the epidemiology, the question is, why?
There are a few theories floating around out there, but most of them focus on antibodies.
An in vitro study of the SARS coronavirus from 2008 found that anti-A antibodies inhibited the ability of the viral spike protein to bind to its receptor, ACE2.
So, a leading theory is that people with blood type O, like me, might be protected if they have some anti-A antibodies floating around.
Of course, people with type B blood also have anti-A antibodies, and we haven't seen protection in them so far.
The other possibility is that the antibodies generated against the virus are cross-reactive with the blood group A antigen, so when someone with blood group A is generating those antibodies, they might also be making antibodies that make their platelets a bit stickier, leading to some of the thrombotic events we've seen in COVID-19 patients. Of course, this doesn't explain why the risk for infection would be higher, only the risk for bad outcome after infection.
I'm left a bit puzzled. Am I convinced that there is something here? Yes—but I'm not sure what it is. Whether it's a direct biologic effect of blood type, or whether blood type is a marker for something else—a nearby gene, for instance—or maybe even socioeconomic status—is ongoing work. As we get more answers, we'll tell you about them here.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale's Program of Applied Translational Research. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @methodsmanmd and hosts a repository of his communication work at www.methodsman.com.
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
"type" - Google News
June 17, 2020 at 02:18AM
https://ift.tt/2Y5lfWw
Is COVID-19 Risk Linked to Blood Type? - Medscape
"type" - Google News
https://ift.tt/2WhN8Zg
https://ift.tt/2YrjQdq
Bagikan Berita Ini














0 Response to "Is COVID-19 Risk Linked to Blood Type? - Medscape"
Post a Comment