

FULL CLAIM: “People with blood type O [are] more protected against COVID-19”; “If a person with blood type A transmits the virus to a person with type O blood, the type O person will have antibodies that can fight the virus.”
REVIEW
An article published in the Jerusalem Post declares that people with type O blood are “more protected against COVID-19”. The article has received more than 23 million views on Facebook and more than 900,000 interactions on the platform since its publication on 15 June. The claim itself had already begun circulating in March 2020 after a preprint (a study that has not yet been peer-reviewed by other scientists) was released by a group of researchers in China. Their study examined blood type prevalence among COVID-19 patients in several Chinese cities, including Wuhan, the original epicenter of the outbreak[1]. The Jerusalem Post article cites this study and others as providing supporting evidence for the claim.
Based on this study, PolitiFact and Snopes fact checked the claim in March 2020; PolitiFact concluded that the study’s findings have not yet been validated and to treat its conclusions with caution, while Snopes found the claim to be unproven. But given that more studies regarding the association between blood type and COVID-19 risk have been published since then, Health Feedback decided to re-examine the newer evidence from four studies cited in the Jerusalem Post article to investigate whether the claim is now substantiated by additional studies. Our analysis finds that the article failed to mention the many caveats and limitations of the recent studies it cites, which exaggerates the certainty and significance of the findings.
1. Zhao et al. MedRxiv[1]
This study formed the basis of the March 2020 claim. It examined blood type prevalence among 1,775 COVID-19 patients (among whom 206 died) at Jinyintan Hospital and 113 patients at Renmin Hospital, both located in Wuhan, Hubei province, as well as 285 patients at Shenzhen Third People’s Hospital, Guangdong province. The prevalence of different blood types among COVID-19 patients was then compared to that of the general population in the respective cities (Wuhan and Shenzhen).
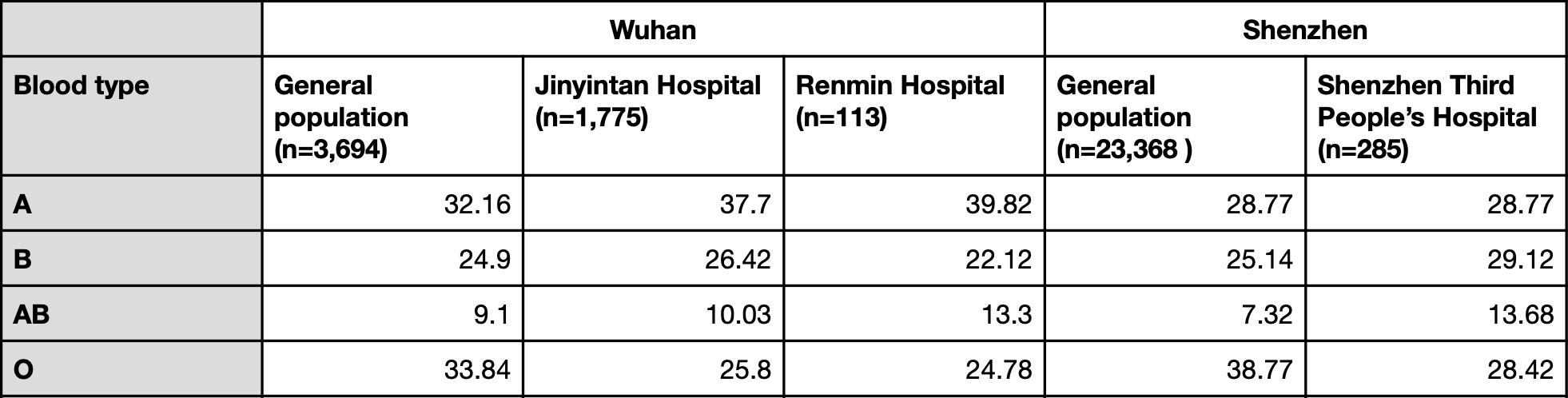
Table 1. Blood type prevalence in the general population and COVID-19 patients in the study (expressed as a percentage).
Based on the differences in blood type prevalence between the general population and hospitalized COVID-19 patients, the authors concluded that the proportion of people with type A blood was significantly higher among COVID-19 patients than in the general population, while the proportion of people with type O blood was significantly lower.
However, looking at the actual figures, we can see that this pattern only holds true in the case of the two Wuhan hospitals, but is not reproduced in the Shenzhen hospital, where blood type AB was overrepresented but blood type A was not. The authors did not explain why this discrepancy was present.
The researchers pointed out that their sample size was small and cautioned that their analysis did not take into account other factors which may influence COVID-19 severity, like pre-existing medical conditions such as chronic obstructive pulmonary disorder, diabetes, and vascular disease.
“It should be emphasized, however, that given the above limitations, it would be premature to use this study to guide clinical practice at this time,” they warned. “Large replication studies with complete information should be encouraged to pursue and are needed to verify the present findings.”
This Mar. 17 article in the South China Morning Post reported comments on the findings in this preprint by a few scientists. Yingdai Gao, a researcher with the State Key Laboratory of Experimental Haematology in Tianjin, said that the findings “may be helpful to medical professionals, but ordinary citizens should not take the statistics too seriously.”
People with type A blood should not panic, she said. “It does not mean you will be infected 100 percent,” she said. “If you are type O, it does not mean you are absolutely safe, either. You still need to wash your hands and follow the guidelines issued by authorities.”
Sakthivel Vaiyapuri, associate professor in cardiovascular & venom pharmacology at the University of Reading, published an article in The Conversation on 24 March 2020, which discussed this preprint’s findings:
“In this observational study, if they considered several other parameters, such as the previous history of other – specifically immune or respiratory-related – diseases, the conclusions might have been different. They have also not explained why they failed to see a significant difference between the blood groups in the Shenzhen hospital. And given COVID-19 is a pandemic, the sample size that they have analysed is not sufficient to draw firm conclusions.”
He warned that more scientific studies were needed to determine the relationship between blood groups and COVID-19. Like Gao, Vaiyapuri also emphasized that people should continue to take precautions to prevent infection, regardless of their blood type.
Tara Moriarty, an associate professor at the University of Toronto who studies infectious diseases, told Snopes that the study provides “an interesting observation that may have an impact on how we identify those most at risk of disease, but until it has been fully peer-reviewed and confirmed/disconfirmed by additional studies, we cannot yet say if blood type affects susceptibility to COVID-19 infection.”
2. Li et al., British Journal of Haematology[2]
This study examined the blood type prevalence of 265 COVID-19 patients at the Central Hospital of Wuhan who had developed pneumonia. Below is the table listing percentages of the prevalence of different blood types at this hospital.
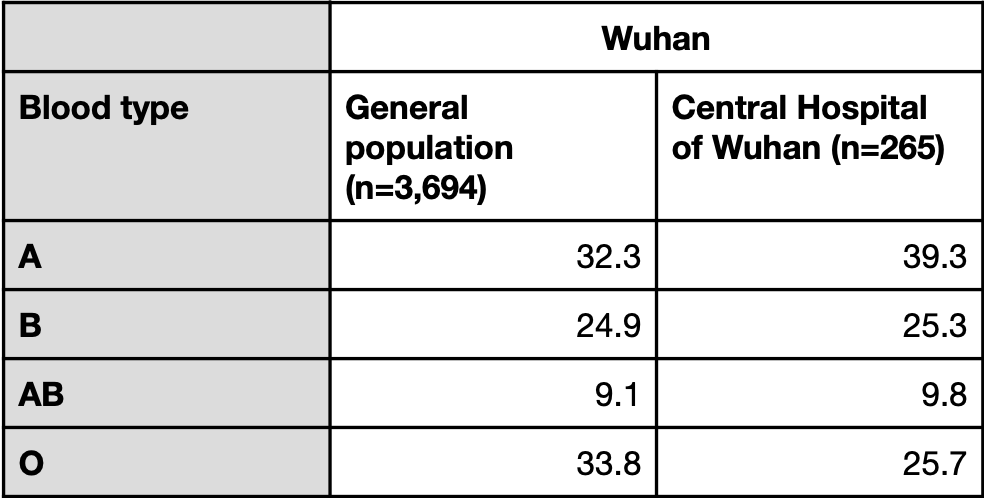
Table 2. Blood type prevalence observed in the general population and COVID-19 patients with pneumonia at the Central Hospital of Wuhan (expressed in percentages).
In its analysis, it also took into account the data from the two Wuhan hospitals in the study by Zhao et al.[1], but not that of the Shenzhen hospital. Unlike the study by Zhao et al., this study did attempt to eliminate confounding factors, such as chronic diseases, although the sample sizes for certain diseases were very small. For example, the authors reported a significantly higher proportion of patients with blood type A who had hepatitis compared to the control group. However, the total number of patients with hepatitis was seven, of which six had blood type A and one had blood type B. Given the very small sample size, the association between blood type A and hepatitis observed in this study may not be meaningful.
The authors concluded that “people with blood group A had a significantly higher risk of SARS‐CoV‐2 infection, whereas blood group O had a significantly lower risk of SARS‐CoV‐2 infection.” However, the sample size for this study is even smaller than in the preprint by Zhao et al., whose findings, as explained earlier, have been called into question by scientists due to its small sample size.
3. Ellinghaus et al., New England Journal of Medicine[3]
This study was conducted in Italy and Spain, involving 1,980 COVID-19 patients from seven hospitals who had been diagnosed with severe COVID-19, which the authors defined as respiratory failure. The researchers conducted a genome-wide association study (GWAS) to identify potential genetic variants associated with the risk of developing severe COVID-19. They found a significant association between severe disease and two different genetic loci (or regions), one of which was located on chromosome 3 and the other on chromosome 9. The region on chromosome 3 spanned six different genes, although the researchers were unable to reliably identify a causative gene with their dataset.
The region on chromosome 9 contains the ABO gene, which codes for an enzyme that converts a protein called the H antigen into A and B antigens. Individuals with blood type O harbor two copies of an ABO gene variant (homozygous) that results in a non-functional enzyme which cannot convert H antigen to A or B antigens. Therefore, people with blood type O cannot produce A or B antigens.
Based on the ABO genotype detected in the GWAS, the researchers inferred the blood type of healthy controls and patients, with the following results:
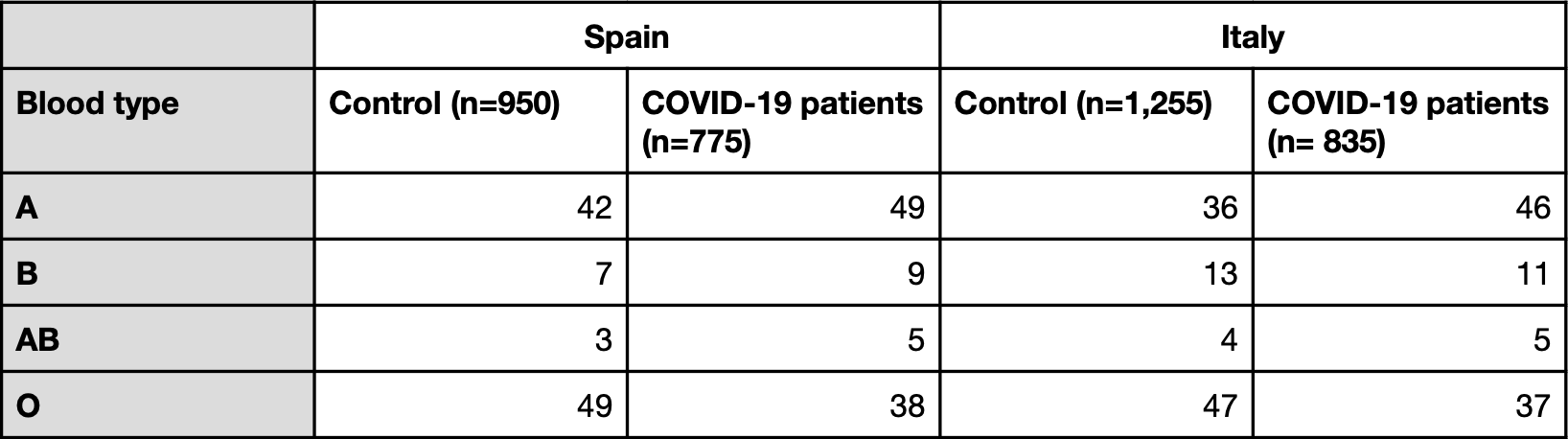
Table 3. Blood type prevalence in the study by Ellinghaus et al. (in percentage)
Similar to what Zhao et al. and Li et al. reported, the blood types showing the greatest differences were A and O, which were more and less represented among COVID-19 patients than in the control population, respectively.
The authors concluded that “Our genetic data confirm that blood group O is associated with a risk of acquiring Covid-19 that was lower than that in non-O blood groups, whereas blood group A was associated with a higher risk than non-A blood groups.”
However, as in the study by Zhao et al., they were not able to adjust for confounding factors such as underlying cardiovascular and metabolic issues associated with COVID-19 risk. And the authors called for more follow-up studies towards identifying potential biological mechanisms and determining the potential of the ABO genotype for profiling COVID-19 risk in patients.
In a CNN report on this study, Roy Silverstein, professor of medicine at the Medical College of Wisconsin and hematologist, said that the blood type link was plausible, but that “the absolute difference in risk is very small” and would not be of much importance to the public in general.
“The risk reduction may be statistically significant, but it is a small change in actual risk. You never would tell somebody who was Type O that they were at smaller risk of infection,” he said.
4. 23andMe
23andMe is a company that offers consumer genetic testing services. In contrast to the earlier studies discussed in this claim review, the company took a more informal approach in reporting its results. It described in a blog post that among more than 750,000 people who had used 23andMe’s genetic testing service and self-reported as COVID-19 positive, “those with the O blood group were 9-18% less likely to test positive compared to the other groups”.
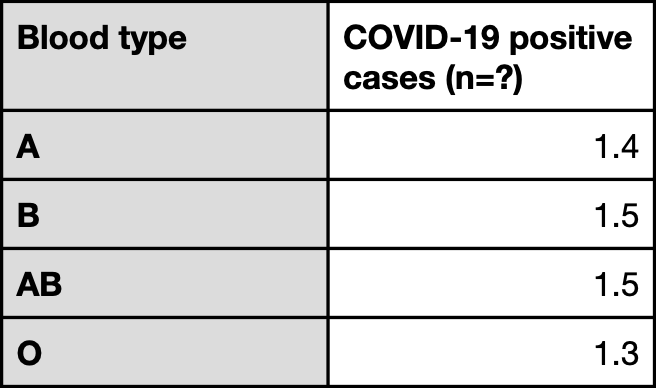
Table 4. Prevalence of different blood types among individuals who used 23andMe’s genetic testing services and had self-reported a positive COVID-19 test (expressed in percentages).
However, unlike the other studies, 23andMe did not sample a representative population that was COVID-19 negative to check the prevalence of different blood types in the general population. In other words, while the company observed a lower percentage of people with blood type O reporting a positive COVID-19 test relative to people with other blood types, it is difficult to determine whether this is simply due to a lower prevalence of blood type O in the sample population. The results have also not been peer-reviewed by other scientists, hence its report should be taken with a pinch of salt.
Fumiichiro Yamamoto, an immunohematologist at the Josep Carreras Leukaemia Research Institute in Barcelona, known for his seminal work on the molecular genetic basis for the ABO blood group, told Chemical and Engineering News (C&EN), a publication by the American Chemical Society, that “it’s hard to say much about the 23andMe results because the company did not publish its data.”
Are there known instances of blood type influencing disease risk?
Yes, blood type has been observed to influence the risk of developing certain diseases. For example, this review details how ABO type has been implicated in higher risk of infection by certain bacteria[4]. The blood type O has also been associated with a greater risk of developing severe cholera[5].
The ABO blood group is the most well-known blood group system, but there are in fact more than 30 other blood group systems involving other proteins. This article in The Conversation by Robert Flower, adjunct associate professor at the University of Sydney and specialist in blood transfusion, discusses the various blood group systems, and how one of these blood groups can be involved in providing protection against a form of malaria:
“A blood group known as Duffy is also associated with infection by another type of malaria (known as Plasmodium vivax). When this protein is absent from the red blood cells, the cells are resistant to infection by the malaria parasite. This protein is absent from the blood cells of 90% of sub-Saharan Africans, conferring malaria resistance on this population.”
What about COVID-19? While the studies we discussed have reported an association between disease severity and blood type, a biological mechanism that explains a causal association is still lacking.
A group of scientists have hypothesized that when SARS-CoV-2 infects a cell to produce more virus, it draws on the human host’s own glycan antigens (including A and B antigens, in the case of people with blood types A, B, and AB) when forming its own glycan shield[6]. Because individuals with type O blood form antibodies against A and B antigens, the scientists propose that these antibodies might enable people with type O blood to fight off infection from SARS-CoV-2 generated by individuals with blood types A, B or AB. However, this hypothesis has not been confirmed yet.
Alternatively, Andre Franke, a molecular geneticist at the University of Kiel in Germany and co-author of the NEJM study, speculated in a New York Times article that the chromosome 9 region, which contains the ABO gene, also contains “an on-off switch for a gene producing a protein that triggers strong immune responses,” which might be involved in the immune system’s response to COVID-19.
But how much protection does type O blood confer against COVID-19? The realities of the COVID-19 epidemic in the U.S. suggest that, in the grand scheme of things, any protection or risk that may be associated with a person’s blood type is outweighed by the presence or absence of other risk factors.
Laura Cooling, professor and associate director of transfusion medicine at the University of Michigan, highlighted in this C&EN article that “the idea that having type O blood is protective doesn’t match up with the COVID-19’s epidemiology in the US. Type O blood is more prevalent among African Americans, yet African Americans have experienced disproportionately high infection rates.”
Indeed, the American Red Cross reports that 51% of African Americans (and 57% of Hispanics) have type O blood, in contrast to 45% of Caucasians, yet racial disparities, in which the African-American and Hispanic communities are disproportionately more affected by COVID-19, have been observed. A Morbidity and Mortality Weekly Report, published by the U.S. Centers for Disease Control and Prevention, has found that ethnic minorities are more likely to be affected by COVID-19: among hospitalized patients, 33% were black, compared to 18% in the community[7]. A study by Millett et al. observed that almost twenty-two percent of U.S. counties, which are disproportionately black, accounted for 52% of COVID-19 diagnoses and 58% of COVID-19 deaths nationally[8].
These observations indicate that blood type alone does not strongly predict COVID-19 protection. As Marcella Nunez-Smith, associate professor and director of the Equity Research and Innovation Center at Yale School of Medicine, pointed out in an NPR report: “African-Americans have higher rates of underlying conditions, including diabetes, heart disease, and lung disease, that are linked to more severe cases of COVID-19.” Furthermore, the African-American community is also often affected by reduced access to quality health care and make up a disproportionately higher number of essential frontline workers, meaning that they are more likely to be exposed to the virus.
Therefore, any protection arising from type O blood might be quite small. “It’s what your blood type is, relative to the other person who exposed you, relative to all the other genetic and acquired health conditions you have,” Cooling said.
Conclusion
In summary, a few studies have reported a lower representation of people with blood type O among COVID-19 cases relative to the general population. Although this finding is intriguing and may eventually be useful for identifying patients at risk of severe disease, there is currently not enough evidence available to determine if a causal association is involved. Some of the studies used to support the claim that type O blood protects against COVID-19 did not take into account certain confounding factors in their analysis, like pre-existing medical conditions, towards COVID-19 risk and severity. Therefore, it is difficult to say how much the findings of these studies were influenced by these factors.
The Jerusalem Post article is misleading, as it does not mention the caveats of the research studies it cites nor does it indicate that the statement “If a person with blood type A transmits the virus to a person with type O blood, the type O person will have antibodies that can fight the virus” is essentially a hypothesis which has not been confirmed yet.
Finally, these studies clearly demonstrate that people with blood type O can and do become infected with SARS-CoV-2, therefore people should continue to take precautions to avoid infection regardless of their blood type. There are many factors that contribute to COVID-19 infection risk and severity, and scientists have warned that any protective effect that blood type O may confer is likely very small, relative to other factors such as pre-existing medical conditions and socioeconomic background.
REFERENCES
"type" - Google News
June 22, 2020 at 07:21PM
https://ift.tt/2B1Dxzd
People should take precautions against COVID-19 regardless of their blood type - Health Feedback
"type" - Google News
https://ift.tt/2WhN8Zg
https://ift.tt/2YrjQdq
Bagikan Berita Ini















0 Response to "People should take precautions against COVID-19 regardless of their blood type - Health Feedback"
Post a Comment