Type 1 diabetes is a disorder in which the immune system inappropriately targets a class of cells in the pancreas known as β cells that produce the hormone insulin, which plays an important role in regulating bloodstream glucose levels and the metabolism of carbohydrates, lipids, and proteins. The loss of insulin causes a range of health problems for people with type 1 diabetes, and patients become dependent on insulin injections for their survival. Even with insulin therapy, people with type 1 diabetes have shortened lifespans and are at an elevated risk of developing myriad complications.
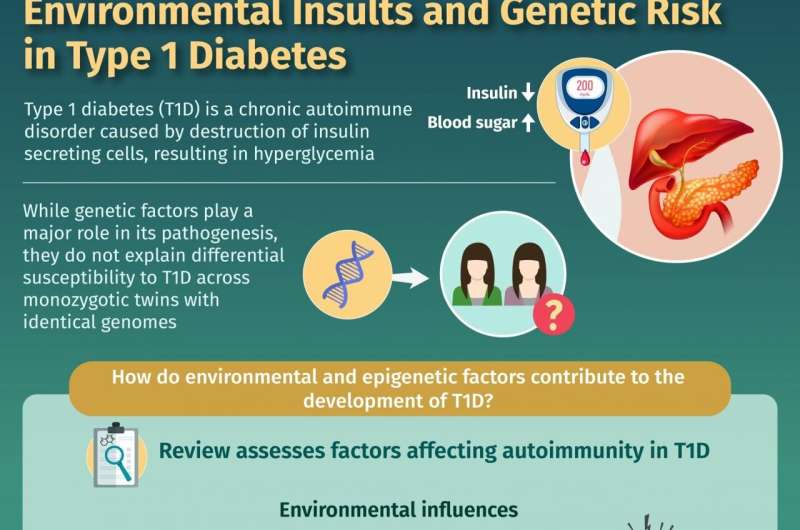
Previous studies have identified numerous genetic risk factors for type 1 diabetes. One notable finding is the importance of the HLA region, a part of the human genome that contains multiple genes and explains approximately 40–50% of the genetic risk for type 1 diabetes. However, studies of identical twins have identified cases in which one twin develops type 1 diabetes while the other twin does not—which indicates that genetic risk factors cannot fully explain the occurrence of type 1 diabetes. This finding is consistent with the known relevance of certain environmental factors. For example, most studies have found that breastfeeding and vitamin D consumption protect against type 1 diabetes and that cow's milk and the early introduction of gluten increase the risk of type 1 diabetes. Furthermore, microbes in the human gut play important roles in human health and digestion, and patients with type 1 diabetes often lack diversity in their gut microbiota.
To explain the risk factors for type 1 diabetes more fully, medical researchers have turned to the field of epigenetics, which studies how environmental and lifestyle factors can influence the expression of genes without altering the underlying DNA sequence. In recent years, various research groups have published studies confirming that epigenetic changes related to environmental conditions contribute to the development of type 1 diabetes. In a review article recently published in Chinese Medical Journal, a team of researchers from the Huazhong University of Science and Technology led by Drs. Cong-Yi Wang and Fei Xiong set out to summarize how epigenetic factors modulate the risks of type 1 diabetes. They also aimed to discuss the potential of these epigenetic factors to serve as markers for monitoring disease progression and as targets for therapeutics.
One important mechanism of epigenetics is DNA methylation, which refers to the presence of chemical tags called methyl groups on DNA. DNA methylation patterns influence whether and how strongly a gene is expressed, and past studies have identified numerous methylation sites that influence the risk of type 1 diabetes. Some of these methylation sites lie within the previously mentioned HLA regions, which is highly relevant to type 1 diabetes. Other methylation sites affect the INS gene, which is second only to the HLA region in terms of influencing the risk of type 1 diabetes.
Another mechanism of epigenetics is chemical modification of histones, which are proteins around which DNA strands are wound. Several studies have reported abnormal histone modification patterns in patients with type 1 diabetes. These modifications may increase the risk of type 1 diabetes by influencing the expression of genes related to inflammation and immunity, and the elevated blood glucose levels associated with type 1 diabetes may also cause abnormal histone modification patterns.
Epigenetic effects can also be expressed in the form of noncoding RNAs, which are RNA molecules that have functional roles other than the standard role of providing instructions for protein synthesis. Noncoding RNAs are a diverse class of genetic molecules, and they can bind DNA, other RNA strands, and proteins. Through their various actions, they can promote or suppress the expression of certain genes. Recent studies have yielded evidence that noncoding RNAs can contribute to type 1 diabetes by influencing the immune system and causing β cell dysfunction.
Dr. Wang says, "Given the relationship between epigenetic changes and type 1 diabetes, various epigenetic changes could serve as markers for disease progression and treatment effects or even as targets for future therapeutics. For example, noncoding RNAs can be measured noninvasively, while changes in DNA methylation levels and patterns for particular genes could indicate that a genetically predisposed person is developing type 1 diabetes." Furthermore, the researchers cite studies that have yielded evidence that drugs that alter DNA methylation could benefit patients with type 1 diabetes.
Dr. Xiong says, "Based on existing literature, it is clear that environmental insult-induced epigenetic changes modulate the expression of critical genes relevant to the initiation and progression of autoimmunity and β cell destruction and are therefore implicated in the development of type 1 diabetes." This information will be valuable to medical researchers who wish to develop new ways to predict the onset of type 1 diabetes, assess the condition's severity and progression, and provide patients with effective treatment options.
Explore further
Provided by Chinese Medical Journal
Citation: Beyond mere blueprints: Variable gene expression patterns and type 1 diabetes (2021, June 18) retrieved 19 June 2021 from https://ift.tt/3j65fi3
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without the written permission. The content is provided for information purposes only.
"type" - Google News
June 18, 2021 at 09:24PM
https://ift.tt/3j65fi3
Beyond mere blueprints: Variable gene expression patterns and type 1 diabetes - Medical Xpress
"type" - Google News
https://ift.tt/2WhN8Zg
https://ift.tt/2YrjQdq
Bagikan Berita Ini














0 Response to "Beyond mere blueprints: Variable gene expression patterns and type 1 diabetes - Medical Xpress"
Post a Comment