Life with type 1 diabetes is a juggling act of diet, exercise, and insulin therapy to maintain normal blood sugar levels. While there's no shortage of solutions in the works for trying to make diabetics' lives easier, a promising new approach focuses on the insulin itself.
Michael Weiss, a biochemist from the School of Medicine at Indiana University in the US, and colleagues have gone back to the drawing board on the insulin molecule, tweaking the structure to respond to the presence of a simple carbohydrate, with the aim of reconnecting the activation of insulin with internal levels of blood sugars again.
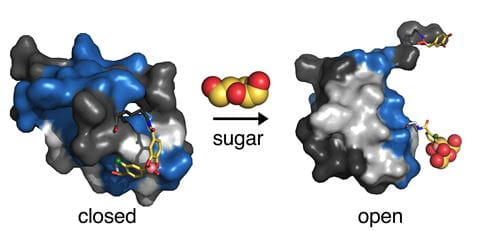
Their modification focuses on a feature already built into the molecule's shape – a protective 'hinge' that allows the protein to function when open, keeping it otherwise stable while closed.
 (IU School of Medicine, 2021)
(IU School of Medicine, 2021)
A new design means the insulin molecule only opens in the presence of a 'key', such as a simple sugar molecule.
The experiments carried out by Weiss and his team used the carbohydrate fructose, showing it was possible to manipulate insulin so it only activated a sample of cells derived from the liver when 'switched on' by the presence of a certain amount of the sugar.
More a proof of concept than a proven therapy, the idea would theoretically work the same for an insulin that's shaped to instead activate in the presence of glucose. The result opens the way for a means of smoothing out much of the guesswork in treating diabetes.
"The promise of this kind of 'smart' insulin is that it would transform diabetes care, so people wouldn't have to worry anymore," says Weiss.
Type 1 diabetes is an autoimmune condition that affects some 15 in every 100,000 people around the world. In effect, the body's immune system destroys cells in the pancreas responsible for measuring out precise amounts of the hormone insulin in accordance with levels of glucose floating about in the blood supply.
Without controlled amounts of insulin being delivered around the body at the right moment, gates that would ordinarily channel glucose into cells remain firmly locked, cutting off the fuel to energy-hungry tissues and organs when they need it most.
For diabetics in centuries gone, this would tragically have meant an early death. Thankfully the fate of millions changed with the discovery that insulin could be purified and injected artificially, crudely doing the pancreas's work on its behalf.
It's an effective remedy, but not one without numerous challenges. The body's hunger for glucose is far from predictable, driving levels up and down seemingly on a whim.
Without enough insulin, blood sugar levels can remain high in a state of hyperglycemia, kicking off a litany of symptoms from excessive thirst to headaches, blurred vision, and fatigue.
Overload your body with insulin and cells quickly gobble up the blood's supply of glucose, leading instead to a state of hypoglycemia. In mild forms, this low sugar level leads to excess sweating, confusion, shakiness, and irritability. In severe forms, hypoglycemia raises the risks of seizures, and occasionally even leads to death.
No matter which way you go, when glucose isn't in good supply the body turns to fat as a source of energy, producing ketones as a waste product. Should these build up in large enough amounts, the result is a potentially dangerous condition called ketoacidosis.
Advances in knowledge and technology have certainly helped individuals manage their sugar levels to avoid tragic outcomes. But transforming the insulin molecule into a biochemical sensor itself could weave in a fail-safe mechanism that makes the hormone ineffective when blood sugar drops below a certain point.
"The reason a glucose-responsive insulin is important is that the biggest barrier to the effective use of insulin, especially in type 1 diabetes, is the fear of the consequences of blood sugar going too low," says Weiss.
The concept is one being explored by other researchers. Last year, a team of scientists from the University of Copenhagen and biotech firm Gubra found success in a similar approach, creating a form of insulin with an attached group that broke apart in the presence of glucose to make the molecule functional.
Shown to function in rats, it's yet another potential automated insulin that could one day be incorporated into treatments.
A lot needs to happen between now and then. While effective in theory, the modified hormone would need to be smart enough to recognize a very specific threshold of glucose.
2021 marks the centenary of the discovery of insulin. In another hundred years, those dealing with the challenges of type 1 diabetes might look back on yet another centenary, one where insulin got a bit of a makeover.
This research was published in PNAS.
"type" - Google News
August 08, 2021 at 07:02AM
https://ift.tt/3iBf5YB
Newly Designed 'Smart' Insulin Could Majorly Improve Type 1 Diabetes Treatment - ScienceAlert
"type" - Google News
https://ift.tt/2WhN8Zg
https://ift.tt/2YrjQdq
Bagikan Berita Ini














0 Response to "Newly Designed 'Smart' Insulin Could Majorly Improve Type 1 Diabetes Treatment - ScienceAlert"
Post a Comment