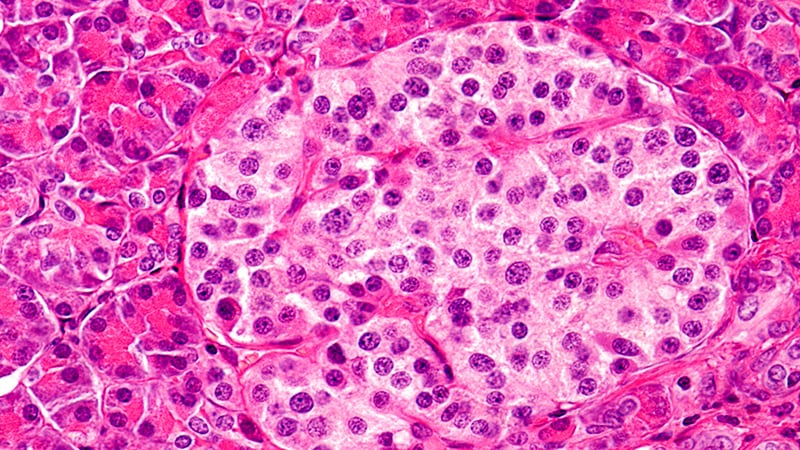
The US Food and Drug Administration (FDA) has approved donislecel (Lantidra, CellTrans Inc), a pancreatic islet cell therapy developed from cadaver donors, for the treatment of people with type 1 diabetes who are unable to achieve target glucose levels owing to severe hypoglycemic episodes.
The product is given as a single infusion via the hepatic portal vein into the liver. A second infusion is given if necessary. Immunosuppression is required to maintain cell viability, just as it is required to support a transplanted kidney or other organ, as these all represent "foreign" tissues to the recipient.
"Today's approval, the first-ever cell therapy to treat patients with type 1 diabetes, provides individuals living with type 1 diabetes and recurrent severe hypoglycemia an additional treatment option to help achieve target blood glucose levels," said Peter Marks, MD, PhD, director of the FDA's Center for Biologics Evaluation and Research, in an FDA statement.
The product was approved despite concerns from the American Society of Transplant Surgeons, the American Society of Transplantation, and an organization of more than 50 transplant surgeons ― the Islets for US Collaborative ― whose members argue that cadaver-derived (allogeneic) pancreatic islets should be regulated as transplanted organs rather than as biologic drugs, as is done in many other parts of the world.
Lantidra differs from stem cell therapy being developed by Vertex Pharmaceuticals. In the latter, beta cells are grown from allogeneic stem cells using a proprietary technology. So far, six patients have received the therapy, and it has been successful in all of them to varying degrees, as reported at last week's American Diabetes Association meeting. So while this is a promising technology, with talk of a "cure" for type 1 diabetes, it's important to remember that this is very early in the development phase, says Anne Peters, MD, of the University of California, Los Angeles, in her latest column for Medscape.
Approval Based on Small Studies, With Adverse Events
The approval of Lantidra, following a 12-4 vote in favor by the FDA's Cellular, Tissue, and Gene Therapies Advisory Committee in April 2021, was based on two nonrandomized, single-arm studies that included a total of 30 individuals with type 1 diabetes who had hypoglycemic unawareness and who received between one and three infusions of donislecel.
Insulin independence was achieved at 1 year by 21 participants; 11 were still insulin independent at 5 years, and 10 remained so more than 5 years. Five participants were unable to discontinue insulin treatment at all.
Adverse events included nausea, fatigue, anemia, diarrhea, and abdominal pain. Most of the participants experienced at least one serious adverse reaction related to the method of infusion and/or the use of immunosuppression. Some of these reactions required discontinuation of the immunosuppressive medications, resulting in the loss of islet cell function and return to insulin dependence.
"These adverse events should be considered when assessing the benefits and risks of Lantidra for each patient. Lantidra is approved with patient-directed labeling to inform patients with type 1 diabetes about benefits and risks of Lantidra," according to the FDA statement.
US Transplant Physicians Had Expressed Concern, Bill Introduced
The transplant surgery organizations had written letters to the FDA, as well as to several other government agencies, to ask that the regulatory framework for Lantidra be shifted from the FDA to the Organ Procurement and Transplantation Network and the United Network for Organ Sharing.
They also wrote to members of Congress. On June 22, 2023, US Senators Mike Lee (R-UT), Ted Budd (R-NC), and Marsha Blackburn (R-TN) introduced the Islet Transplantation Bill, which would shift the regulatory framework for cadaveric islets from that of biologic drugs to transplanted organs.
Asked for comment, Piotr Witkowski, MD, PhD, the leader of the Islets for US Collaborative, told Medscape Medical News, "We were really happy about the introduction of the islet bill. Now, we're concerned about negative downstream effects of granting a licence to a private company for distribution of the cadaveric islets."
During the FDA's Cellular, Tissue, and Gene Therapies Advisory Committee's discussion in 2021, several panel members noted that the target patient population for this treatment with the current indication will likely be smaller today than it was when the two studies were initiated, in 2004 and 2007, given current automated diabetes technology ― such as insulin pumps, continuous glucose monitors, and hybrid closed-loop systems in which the two are linked together as a so-called artificial pancreas ― that reduces hypoglycemia risk.
Miriam E. Tucker is a freelance journalist based in the Washington DC area. She is a regular contributor to Medscape, with other work appearing in the Washington Post, NPR's Shots blog, and Diabetes Forecast magazine. She is on Twitter @MiriamETucker.
For more diabetes and endocrinology news, follow us on Twitter and Facebook.
"type" - Google News
June 29, 2023 at 08:22PM
https://ift.tt/5HsT9KJ
FDA OKs Pancreatic Islet Cell Therapy for Type 1 Diabetes - Medscape
"type" - Google News
https://ift.tt/9Ee4JMD
https://ift.tt/3BUKxZk
Bagikan Berita Ini














0 Response to "FDA OKs Pancreatic Islet Cell Therapy for Type 1 Diabetes - Medscape"
Post a Comment